Let’s Adopt Another Country’s Immunisation Schedule and Call it Shared Decision Making – What Could Possibly Go Wrong?
Listen to the audio file for the essentials.
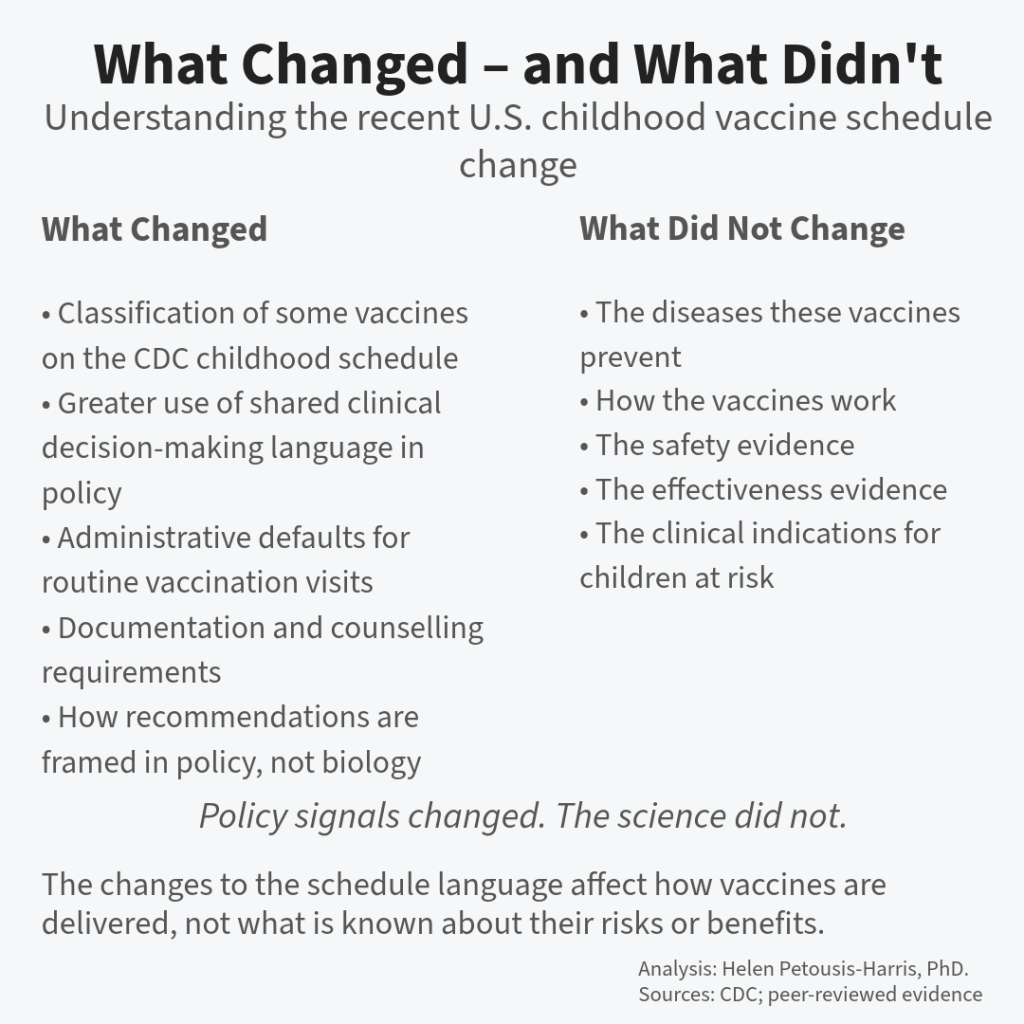
Public debate has treated recent changes to the U.S. childhood vaccine schedule as a scientific shift and called it shared decision making. It isn’t. What’s changed is how policy is framed and operationalised—while the underlying evidence, disease risks, and vaccine performance remain the same.
Same suit. Different body. Predictable results.
The last week has been disorienting for anyone who works in, reports on, or depends upon childhood immunisation policy. In a matter of days, six familiar vaccines in the US immunisation schedule quietly moved from “routine” to “optional,” framed not as a reversal but as a refinement: a shift toward “shared clinical decision-making.” What is good for Denmark must be good for the US, right? Actually, I really doubt that is the motivation, but let’s focus on how utterly insane this is for public health.
On the surface, this may look like yet another chapter in America’s long, noisy vaccine argument. It isn’t. What makes this moment different is not new science, nor a newly discovered risk, nor even a novel ideological claim. It is structural. Structural changes have downstream effects that persist long after the headlines fade. Many infants and children will pay the ultimate price with their lives.
What changed was not the evidence base. What changed was the default.
That distinction matters far more than most commentary has acknowledged.
What Actually Changed (and What Did Not)
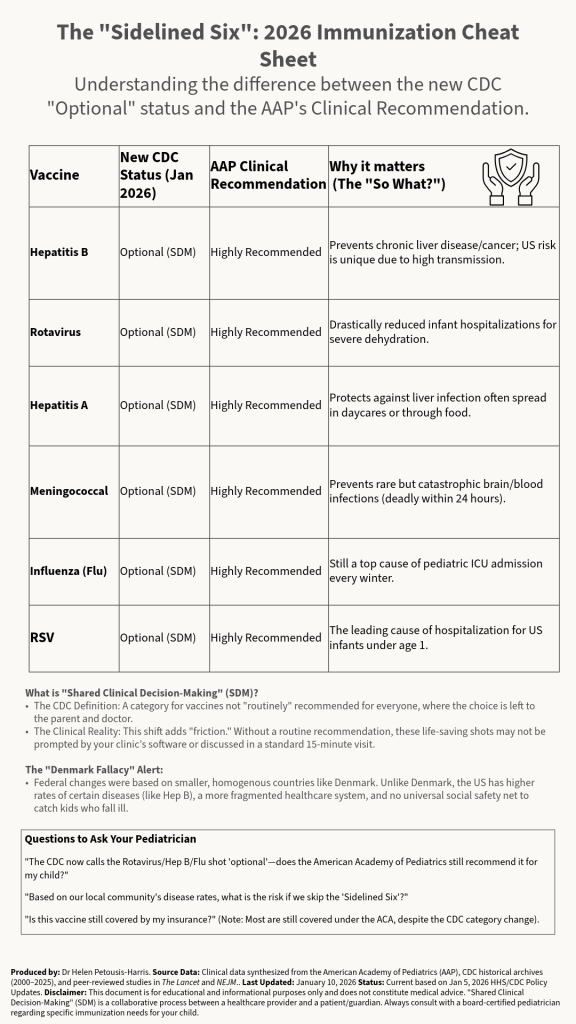
The policy shift itself is straightforward. Six vaccines — Hepatitis A, Hepatitis B, Rotavirus, Influenza, RSV, and Meningococcal — were removed from the list of universally recommended childhood immunisations and placed under “shared clinical decision-making” (SDM).
What did not change is equally important. The underlying clinical evidence supporting these vaccines has not been withdrawn, revised, or contradicted by new safety signals. No new trial overturned prior findings. No surveillance system detected an emergent population-level harm. The scientific substrate remained static.
Shared clinical decision-making is also not new. It has long been used appropriately for interventions where individual values, preferences, or risk tolerance meaningfully alter the balance of benefit and harm — prostate cancer screening is a canonical example. SDM is a process tool, not a warning label.
The problem is not the existence of SDM. It is its redeployment, or more bluntly, weaponisation.
In practice, SDM is being read by parents, by some clinicians, and increasingly by the public as a signal that the vaccines in question now sit in a grey zone of questionable necessity. That inference is incorrect, but it is predictable and understandable.
When defaults change, behaviour follows. And let’s be honest, the vaccine trust landscape is currently a basket case thanks to gross incompetence and mismanagement.
Why This Narrative Is Gaining Traction
Three rhetorical moves have given the “Great Sidelining” narrative unusual velocity.
First is the appeal to international moderation. The policy has been framed as bringing the U.S. “into alignment with peer nations,” most commonly Denmark. This comparison feels sober, evidence-driven, and reassuringly un-American in tone. It implies restraint rather than retreat. Comparing the US to Denmark because they both have flags with stripes is like comparing a Great Dane to a Chihuahua because they both have four legs and an interest in your sandwich.
Second is the invocation of parental empowerment. “Shared decision-making” sounds like a corrective to paternalism, a restoration of agency rather than a withdrawal of protection.
Third is the language of consensus. By narrowing the schedule to “core” vaccines, the policy implies that what remains is indisputable — and that what was removed is, by contrast, debatable.
Each of these moves is rhetorically effective because each is individually reasonable. Together, they create a powerful but misleading gestalt: that scientific uncertainty has increased, and that discretion is therefore prudent. In other words, it is difficult to understand by simply analysing the individual components.
The science did not move. The framing did.
The Gaps Current Responses Are Missing
Most institutional responses have focused on defending the evidence base. This is necessary but insufficient.
The Scientific Gap: The Denmark Fallacy.
Comparisons to Denmark collapse under minimal scrutiny, but few explanations have been offered in plain language. Disease epidemiology differs. Health system architecture differs. Social safety nets differ. Hepatitis B risk, for example, is shaped by migration patterns, perinatal screening uptake, and household transmission dynamics that are not interchangeable across countries. “Europe does it differently” is not an argument; it is a starting point for context that has largely gone unexplained. Here are some examples of the striking differences between these two countries.
First, the burden of acute hepatitis B in Denmark is a fraction of what it is in the US.
Notes on the chart.
This is acute hepatitis B, not chronic infection and not overall HBV prevalence. (Denmark’s HBV notifications include chronic cases too; we’re explicitly using the acute subset from SSI.) SSI+2SSI+2
Cross-country comparisons are always imperfect because surveillance systems + testing patterns differ; the point of this chart is the order-of-magnitude gap, not micrometre-level precision. (Also: 2020 is a weird year for almost everything.)
The communication gap: what SDM actually looks like.
In theory, SDM is a structured conversation supported by decision aids, time, and continuity of care. In reality, it is being introduced into 15-minute paediatric visits that are already compressed by administrative burdens. Without clear tools, SDM degrades into deferral. Deferral becomes delay. Delay becomes non-vaccination. None of this requires ideological opposition — only friction. I suppose it serves to ensure fewer people are vaccinated, which is the goal of the pro-disease individuals now leading US public health.
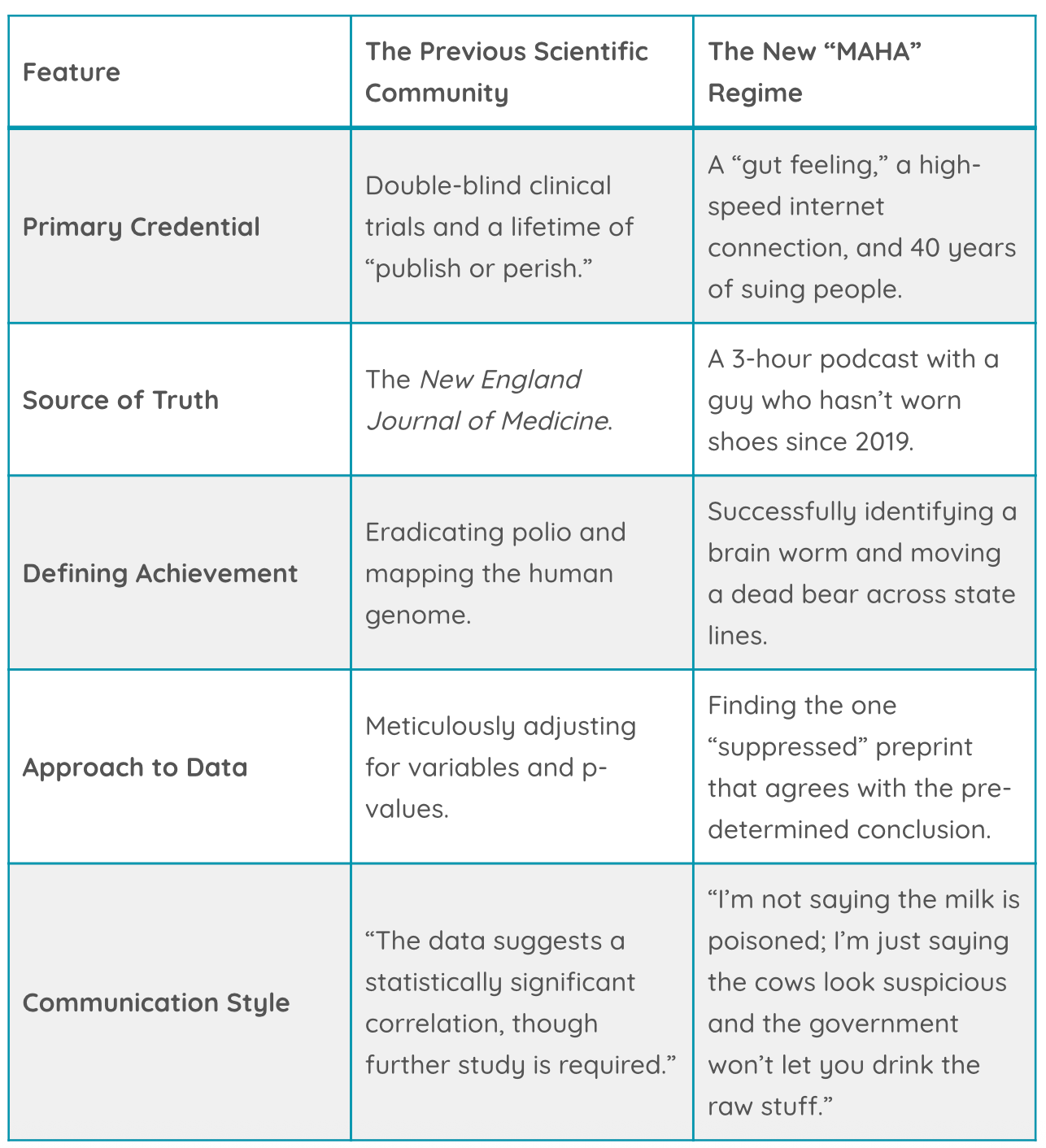
The credibility gap: institutional displacement.
Because the policy originates from within Centers for Disease Control and Prevention, medical societies now find themselves publicly counter-positioned against the lead federal health authority. To the public, this does not read as healthy debate; it reads as expert disagreement. When experts disagree, people default to inaction. There is deeply false equivalence going on here, the global community of scientists and clinicians versus… whatever the new regime is.
This is not a failure of messaging discipline. It is a predictable outcome of institutional misalignment.
How Vaccine Avoidance Increases Without Misinformation
No conspiracy is required for harm to emerge here.
Administrative complexity increases. Clinicians face longer conversations without better tools. Parents encounter ambiguity where there was once clarity. The psychological cost of decision-making is transferred downward — from systems to individuals.
Behavioural science has repeatedly documented this pattern. When the burden of choice increases, uptake decreases, even among those who are not opposed in principle. This is not hesitancy driven by fear; it is avoidance driven by overload.
The policy’s stated goal is trust. Its likely mechanism is attrition.
What Would Actually Help Right Now
Arguing about reversal is unlikely to help clinicians or families in the near term. What is missing is operational support.
If SDM is now the framework, it needs scaffolding.
What would add immediate value is a set of concise, data-anchored risk profiles for each of the sidelined vaccines — not slogans, not reassurances, but context. Why Hepatitis B vaccination in infancy still matters in a country with variable prenatal screening uptake. Why rotavirus remains a leading cause of hospitalisation in infants despite improvements in sanitation. Why influenza risk is not evenly distributed across children. Why RSV protection changes health-system load, not just individual outcomes.
These are not political arguments. They are clinical ones.
A one-page decision aid per vaccine — something a clinician can put on the table — would do more to support informed consent than any press release. It would also anchor SDM in evidence rather than implication.
The Bottom Line
This moment will likely be remembered, inaccurately, as a scientific debate about vaccines. It is not. It is a systems problem masquerading as a choice problem.
Nothing about the biology changed. What changed was the signal sent by the schedule, and signals shape behaviour whether we intend them to or not.
If the downstream effects are missed vaccinations, it will not be because parents were misled by fringe claims or because clinicians abandoned evidence. This is because ambiguity was introduced without the necessary infrastructure to manage it.
Six months from now, the noise will have faded. The administrative friction will remain. And the consequences will be quietly attributed elsewhere.
Understanding that now is the first step to mitigating what comes next — calmly, precisely, and without pretending that this was ever just another vaccine debate.
References & Further Reading
Primary Policy Documents
HHS Official Press Release (Jan 5, 2026): CDC Acts on Presidential Memorandum to Update Childhood Immunization Schedule. The official announcement detailing the move to “Shared Clinical Decision-Making” (SDM).
CDC Decision Memorandum: Adopting Revised Childhood and Adolescent Immunization Schedule. The technical document signed by Acting Director Jim O’Neill outlining the new categories.
Medical Community Rebuttals
American Academy of Pediatrics (AAP): AAP Opposes Federal Health Officials’ Unprecedented Move to Remove Universal Childhood Immunization Recommendations. The definitive statement labeling the shift “dangerous and unnecessary.”
American Medical Association (AMA): AMA Statement on Changes to Childhood Vaccine Schedule. A critique of the lack of transparency and evidence-based process in the new guidelines.
Infectious Diseases Society of America (IDSA): Medical Groups’ Challenge to Kennedy-backed Vaccine Policies Can Proceed. Report on the legal action taken by leading medical groups against the HHS.
Analysis of the “Denmark Fallacy”
KFF Quick Take: Do We Want to Outsource U.S. Vaccine Policy to Denmark?. An analysis of the fundamental differences in disease epidemiology and healthcare infrastructure between the US and Denmark.
CIDRAP Viewpoint: The Myth of an Over-Vaccinated America. A deep dive into global consensus versus the specific outliers in the Danish schedule.
Impact on Clinical Practice
CIDRAP Op-Ed: Quiet Dismantling: How ‘Shared Decision-Making’ Weakens Vaccine Policy. A critical look at how the administrative “friction” of SDM reduces uptake without formal mandates.
BMJ News: RFK Slashes US Vaccines for Children as Medical Groups Threaten Legal Action. International coverage of the structural changes to the US schedule.
The post Let’s Adopt Another Country’s Immunisation Schedule and call it shared decision making – What Could Possibly go wrong? appeared first on Diplomatic Immunity.